Lung pattern
Normal lung anatomy
Assigning a radiographic abnormality to a specific lung lobe is crucial to be able to narrow down the list of differential diagnoses.
Do you remember the normal anatomy of the canine and feline lung and which lung lobes form the cranio-ventral, which ones the caudo-dorsal lung field?
The canine and feline lung consists of 6 lung lobes. Lobar anatomy is based on the bronchial division. The right lung consists of the following lung lobes:
- Lobus cranialis pulmonis dextri (right cranial lung lobe)
- Lobus medius pulmonis dextri (right middle lung lobe)
- Lobus caudalis pulmonis dextri (right caudal lung lobe)
- Lobus accessorius pulmonis dextri (accessory lung lobe)
The left lung consists of only two lung lobes:
- Lobus cranialis pulmonis sinistri divided into a Pars cranialis and a Pars caudalis (left cranial lung lobe)
- Lobus caudalis pulmonis sinistri (left caudal lung lobe)
Both cranial lung lobes and the right middle lung lobe form the cranio-ventral lung field.
The right and left caudal lung lobe are assigned to the caudo-dorsal lung field.
The perihilar lung field consist of the caudo-dorsal areas of both cranial lung lobes, the dorsal area of the right middle lung lobe, the cranio-ventral areas of both caudal lung lobes and the cranial area of the accessory lung lobe.
A peripheral distribution refers to the periphery, meaning the subpleural region, of each lung lobe. Thus, a peripheral change can be present in the middle of the radiograph, as long as this region corresponds with a lobar border.
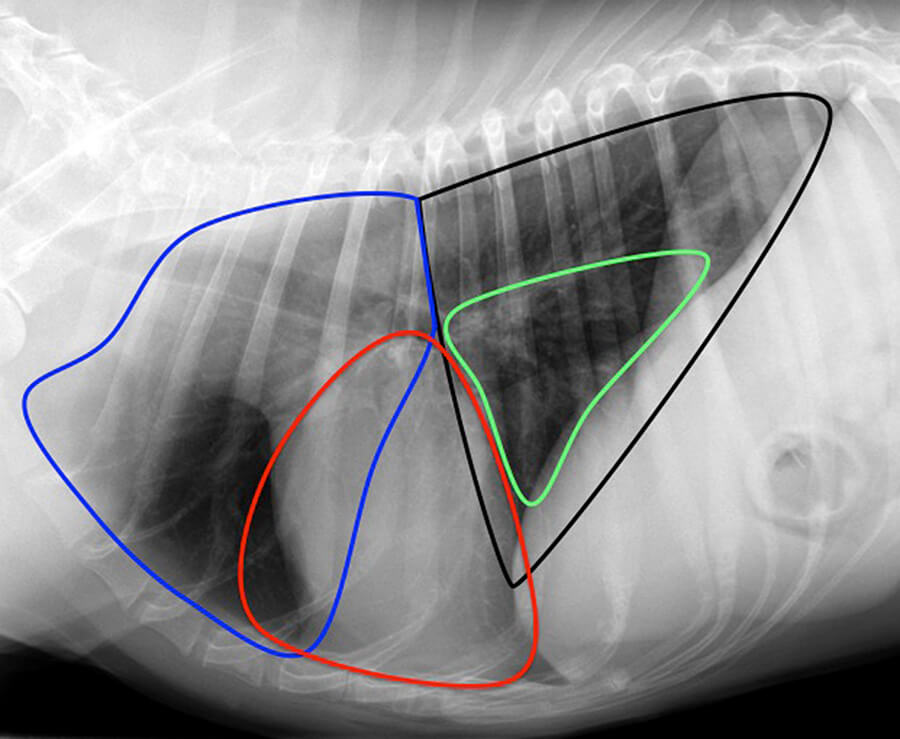
On the following images the approximate border of the different lung lobes is outlined. Legend: blue = right cranial lung lobe; red = right middle lung lobe; green = accessory lung lobe; black = caudal lung lobes (right and left side); solid white line = cranial part of the left cranial lung lobe; dashed white line = caudal part of the left cranial lung lobe
Alveolar, interstitial or maybe bronchial!
Who hasn’t experienced this: you look at a thoracic radiograph and somehow you do see a bit of every lung pattern. Finally you end up with a diagnosis of bronchio-interstitial lung pattern with alveolar infiltrates (mixed lung pattern). To come to a final diagnose based on this description is almost impossible.
But which description translates into a radiological lung pattern.
As for all other regions, the first step in evaluating the radiograph is to look at the technical quality of the radiograph and patient related factors.
- Has the correct exposure setting and algorithm been chosen?
- Is the patient emaciated or obese?
- Has the radiograph been taken during inspiration or exspiration?
In contrast to other body regions the phase of respiration has a significant influence on the radiologic appearance of the lung.
Obesity, exspiration and underexposure lead to an artificial increase in lung opacity. Contrary to that emaciation, deep inspiration and overexposure decrease the lung opacity. If in doubt repeating radiographs may be helpful.
Based on the answers to the above questions you need to decide if the lung of your patient is abnormal.
It is not about deciding if the lung changes you are dealing with are alveolar, interstitial or bronchial. Start with answering the following questions:
Is the lung opacity
- increased?
- decreased?
- normal?
Are the changes affecting the entire lung or are the changes more pronounced in certain areas.
The alveolar lung pattern
The key to diagnose an alveolar lung pattern is the lung vasculature. Their visibility or better loss of their visibility determines if the changes being alveolar or not.
In the altered lung area
- you don’t see lung vessels any more,
- you do see air bronchogramms (dark lines on a white background), mirroring the normal appearance of the lung (white lines on a dark background)
You are done! The lung pattern you are dealing with is an alveolar lung pattern.
Contrary to the other lung patterns a typical distribution helps to choose the most likely diagnosis from the long list of differential diagnosis for an alveolar lung pattern. A list of most likely differential diagnoses based on distribution can be found under the link “DDx alveolar pattern”. In your final diagnosis also consider history, other clinical signs and the result of other diagnostic tests.
Bronchial lung pattern
Bronchial lung changes can be divided into three groups.
- Mineralisation/sclerosis of bronchial walls or bronchial glands
- Soft tissue thickening of the bronchial walls
- Bronchiectasis/ dilatation of bronchi
Mineralisation or sclerosis of the bronchi is usually not difficult to detect. They can delineate the bronchial walls appearing as thin lines or present as cauliflower- like patches. For differential diagnoses check under the following link “DDx bronchial pattern”.
Soft tissue thickening of the bronchial walls can be the result of
- peribronchial infiltrate, (accumulation of cells or fluid around the bronchi)
- accumulation of mucus in the lumen if the bronchi
Lung vessels are still visible, the lung shows “tram lines” and/or “doughnuts”.
— Easier said than seen —
Hint: at first glance, the lung may look as if multiple small nodules are present. Close inspection shows that a small black dot is visible centrally in most of the nodules. Or the lung appears as if a net is spread over it. On close inspection the lines, causing the netlike appearance, run parallel to each other over some distance. For differential diagnoses check under the following link “DDx bronchial pattern”.
Bronchiectasis can be difficult to detect. In general bronchi should decrease in size from the principle bronchi to the periphery. In bronchiectasis a bronchus shows an increased diameter peripherally compared to a more centrally located part. Occasionally the lung parenchyma may appear bullous. For this type of bronchial pattern you will also find a list of differential diagnoses under the following link “DDx bronchial pattern”.
Interstitial lung pattern
Just as for bronchial lung pattern the interstitial lung pattern can be subdivided further
- nodular/ structured
- retriculonodular/ miliary
- unstructured
A nodular or structured interstitial pattern does usually not pose a diagnostic challenge, as one single or multiple soft tissue opaque nodules are visible. The list of differential diagnoses is short and identical to the list for soft tissue opaque nodules in other regions of the body.
In a miliary or reticulonodular lung pattern the radiograph looks as if a snowstorm is blustering. You see multiple, small nodules less than 5mm in diameter.
The unstructured interstitial lung pattern is the most challenging and most over-diagnosed lung pattern. The lung appears as if a white screen door is superimposed onto it. The lung vessels are still outlined.
Before you diagnose an unstructured interstitial lung pattern lean back and reconsider: Is the lung opacity really increased? Is the increased opacity really not related to underexposure, exspiration or any other artefacts causing an increased lung opacity. The list of differential diagnoses is long. You find a list of differential diagnosis under “DDx interstitial pattern”.